AI in brain cancer prediction is revolutionizing how we approach the diagnosis and management of pediatric gliomas, particularly in anticipating cancer relapse. A recent Harvard study demonstrated the superiority of AI tools in evaluating multiple magnetic resonance imaging (MRI) scans over time, providing more accurate predictions of relapse risk compared to traditional methods. Pediatric gliomas, while typically treatable, present unique challenges for clinicians due to their varying likelihood of recurrence, making such advancements critical. By employing innovative techniques like temporal learning in AI, researchers are paving the way for enhanced brain cancer treatment protocols and improved patient care. The implications of this technology could transform the landscape of pediatric cancer treatment, offering less invasive and more tailored approaches for young patients.
Artificial intelligence in oncology, particularly for forecasting brain tumor relapses, is becoming increasingly vital in healthcare. This innovative field harnesses the power of data-driven algorithms to interpret numerous magnetic resonance imaging scans—an evolution in the way medical professionals assess risks associated with conditions such as pediatric gliomas. By utilizing advanced techniques, such as temporal learning, AI systems can now track changes over time, which significantly improves the accuracy of cancer relapse predictions. This approach not only enhances the precision of monitoring patients, but also has the potential to optimize brain cancer treatment by enabling clinicians to make informed decisions based on a patient’s specific risk profile. As this technology evolves, it promises to alleviate the burden on families and health professionals alike by streamlining follow-up procedures.
Understanding Pediatric Gliomas and Recurrence Risks
Pediatric gliomas are a form of brain cancer that primarily affects children and can often be treated successfully with surgical interventions. However, the nature of these tumors varies, leading to different recurrence risks among patients. It’s crucial for healthcare providers to identify which patients are more likely to experience relapse post-treatment to tailor their care strategies effectively. Research indicates that advancements in imaging and artificial intelligence are pivotal in predicting these recurrence risks accurately, transforming the outlook for affected families.
The process of monitoring children who have undergone treatment for gliomas generally involves extensive follow-up care, including regular magnetic resonance imaging (MRI) scans, which can be both stressful and burdensome. Traditional prediction methods have struggled with accuracy, sometimes leading to anxiety for families as they await results. Consequently, harnessing innovative tools, like AI in brain cancer prediction, becomes essential in helping both patients and physicians navigate the complexities of cancer management and potentially spare low-risk patients from unnecessary procedures.
The Role of AI in Brain Cancer Prediction
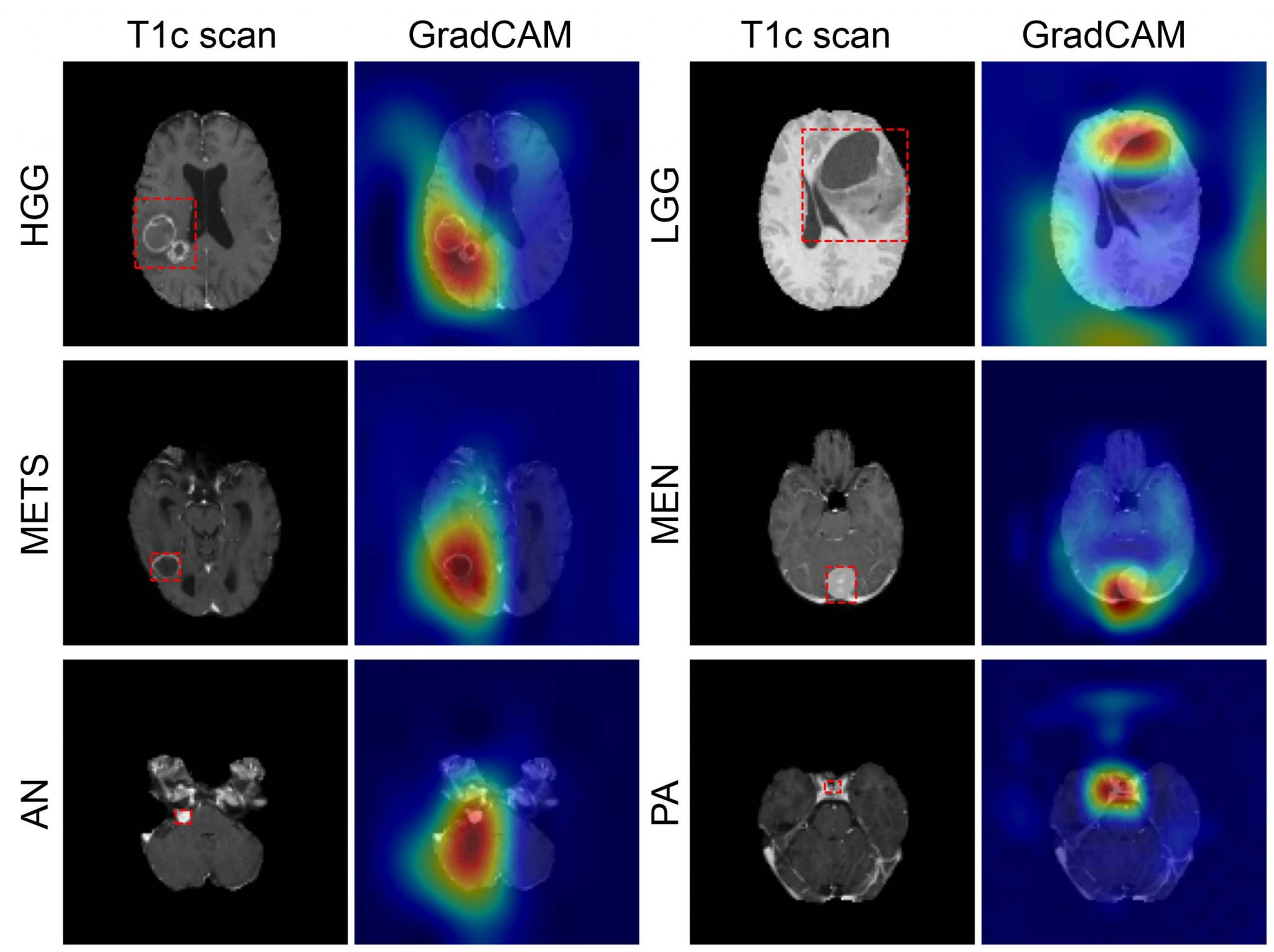
Artificial Intelligence has emerged as a game-changer in the realm of medical imaging, particularly in predicting brain cancer outcomes. Specifically, the integration of AI tools in analyzing multiple brain scans over time allows for a nuanced understanding of tumor behavior and recurrence likelihood. By employing a technique known as temporal learning, AI can detect subtle changes in patient scans that may indicate the impending return of cancer, thereby providing a crucial edge over conventional predictive models that rely on isolated images.
Studies have shown that AI-driven approaches can enhance the accuracy of cancer relapse predictions significantly. With reported accuracies of 75-89 percent for predicting glioma recurrence, the potential for AI to assist in clinical decision-making is immense. This progress not only helps in anticipating which children may need more intensive surveillance or therapy but also encourages a more personalized approach to brain cancer treatment, leading to improved patient outcomes and quality of life.
Innovations in Temporal Learning for Cancer Relapse Prediction
Temporal learning represents an exciting frontier in medical AI applications, particularly for conditions like pediatric gliomas, where the timing and sequence of treatment are critical. By training AI models on a series of consecutive MRI scans taken after surgery, researchers have developed a method that allows algorithms to learn how a patient’s condition evolves over time. This innovative approach captures intricate patterns that single-image analyses might overlook, thereby delivering more reliable predictions regarding the risk of tumor recurrence.
The implementation of temporal learning in predicting cancer relapse has the capacity to revolutionize standard monitoring practices. As highlighted in recent studies, providing AI systems with serial scans enables them to better correlate observable changes with clinical outcomes such as relapse. This can transform patient management strategies, allowing healthcare providers to identify high-risk individuals more effectively and optimize follow-up care, thereby balancing the need for attentive monitoring with the emotional well-being of young patients and their families.
Impact of Enhanced Imaging Techniques in Treatment Plans
Improved imaging techniques, particularly MRI advancements, are instrumental in cancer management and treatment planning. For pediatric glioma patients, precise imaging plays a vital role in determining the effectiveness of interventions and surveilling potential recurrences. The ability to assess tumors accurately through comprehensive imaging allows medical professionals to tailor treatment plans that best fit the patient’s unique situation, improving overall outcomes and potentially reducing the frequency of invasive procedures.
When combined with AI methodologies, enhanced imaging techniques offer even greater predictive power regarding cancer relapse. This combination allows for a more dynamic monitoring approach, facilitating timely adjustments in treatment protocols which can be critical in managing pediatric gliomas effectively. By utilizing this cutting-edge technology, clinicians can strive towards more successful long-term management strategies that ultimately aim to minimize distress for children and their families during a challenging time.
The Future of AI in Pediatric Oncology
The future of pediatric oncology is poised for significant transformation, largely due to the continued integration of artificial intelligence and advanced imaging techniques. As researchers build on findings from studies utilizing AI in brain cancer prediction, we can expect the development of more sophisticated tools that assist in diagnostics, treatment strategy formulation, and monitoring outcomes post-therapy. This paradigm shift aims to create a healthcare environment where data-driven insights lead to more effective, personalized care.
Moreover, with ongoing validation and clinical trials set to test AI-informed predictions, the potential for AI to streamline processes in pediatric cancer care is vast. The goal is not only to improve prediction accuracy but also to enhance patient experiences by reducing the burden of unnecessary imaging and overtreatment. As this technology evolves, it will undoubtedly play a crucial role in shaping the landscape of brain cancer treatment for younger patients, ensuring better health outcomes and improving survivorship rates.
Challenges in Implementing AI and Imaging Techniques
Despite the promising advances in AI and imaging for brain cancer prediction, several challenges remain in their widespread implementation. One significant obstacle involves the integration of AI tools into existing healthcare systems, which can be resource-intensive and require extensive training for healthcare providers. Additionally, ensuring that AI models are robust enough to handle diverse patient populations is crucial, as these tools must be validated across different settings and tumor types to ensure their effectiveness.
Moreover, ethical considerations surrounding AI in medicine, including data privacy and the need for clear guidelines on AI’s role in clinical decision-making, present further challenges. As the adoption of AI becomes more prevalent in pediatric oncology, it is essential to establish frameworks that secure patient information and optimize the use of AI, ensuring that benefits are universally accessible and that families can trust in the technology guiding their child’s care.
The Role of Collaboration in Advancing AI Research
Collaborative efforts among leading research institutions are pivotal in advancing the field of AI for brain cancer prediction. Partnerships, such as those between Mass General Brigham, Boston Children’s Hospital, and other notable entities, harness the expertise and resources required to gather large sets of imaging data, which are essential for training AI models effectively. This collaborative approach not only speeds up research but also enhances the quality and applicability of findings in real-world clinical scenarios.
Sharing knowledge and resources across institutions can lead to significant advancements in understanding the complexities of pediatric brain tumors. By pooling data and expertise, researchers can refine AI tools faster, increasing the accuracy of cancer relapse predictions and uncovering new insights into treatment efficacy. Ultimately, these collaborative efforts will ensure that children with brain cancer receive the most informed and effective care possible.
Preparing for Clinical Trials of AI-Driven Prediction Models
As research progresses, the next crucial step involves preparing for clinical trials that will assess the applicability of AI-driven prediction models in real-world settings. These trials will be essential in verifying the efficacy of AI in improving outcomes for pediatric glioma patients and determining how these tools might influence standard care protocols. Preparing for these trials requires rigorous planning and compliance with ethical standards to ensure the safety and rights of child participants and their families.
Moreover, successful clinical trials could pave the way for the integration of AI systems in routine hospital practices, thereby changing the paradigm of follow-up care in pediatric oncology. With evidence supporting the predictive power of AI, healthcare systems may begin to adopt these technologies more widely, ultimately leading to enhanced patient care, reduced burdens on families, and a more proactive approach to managing pediatric brain cancer treatments.
Looking Ahead: The Legacy of AI in Pediatric Cancer Care
The legacy of AI in pediatric cancer care is just beginning to unfold, particularly regarding brain cancer like pediatric gliomas. The innovations driven by AI research not only hold the potential for transforming predictive accuracy but also aim to instill greater confidence in treatment decisions among healthcare providers and families alike. As the technology matures, it is expected that the long-term impact on survival rates and quality of life for children battling these cancers will be profound.
Eventually, the goal is to create a synergistic relationship between human expertise and AI capabilities, paving the way for a future where predictive modeling becomes a standard part of cancer care. By continuing to innovate and refine these approaches, stakeholders in the healthcare community can ensure that children facing the challenges of brain cancer receive timely interventions tailored specifically to their needs, building a brighter future for pediatric oncology.
Frequently Asked Questions
How does AI in brain cancer prediction improve outcomes for pediatric gliomas?
AI in brain cancer prediction enhances outcomes for pediatric gliomas by accurately predicting the risk of relapse through advanced analysis of multiple MRI scans over time. This is especially critical as early identification of at-risk patients allows for timely interventions, potentially improving treatment effectiveness.
What role does magnetic resonance imaging play in AI in brain cancer prediction?
Magnetic resonance imaging (MRI) is crucial in AI in brain cancer prediction as it provides detailed brain scans that the AI analyzes for patterns indicative of cancer relapse. The use of sequential MRIs allows AI tools to apply temporal learning, increasing prediction accuracy for pediatric gliomas.
Can AI accurately predict cancer relapse in pediatric gliomas compared to traditional methods?
Yes, AI demonstrates superior accuracy in predicting cancer relapse in pediatric gliomas compared to traditional methods. In recent studies, AI models utilizing temporal learning achieved prediction accuracies of 75-89%, significantly outpacing the approximate 50% accuracy associated with traditional single-scan evaluations.
What is temporal learning in AI for brain cancer prediction?
Temporal learning in AI for brain cancer prediction refers to a method where the AI learns from multiple MRI scans taken over time. This approach enables the AI to recognize subtle changes in the brain’s condition post-surgery, thereby improving its ability to predict the likelihood of cancer recurrence.
How can AI in brain cancer prediction change treatment plans for pediatric glioma patients?
AI in brain cancer prediction can transform treatment plans for pediatric glioma patients by providing more accurate assessments of recurrence risk. This allows doctors to tailor follow-up imaging schedules—reducing unnecessary stress for low-risk patients while ensuring high-risk patients receive timely interventions.
Why is improving AI in brain cancer prediction important for families dealing with pediatric gliomas?
Improving AI in brain cancer prediction is vital for families as it reduces the number of stressful MRI sessions required, providing a clearer understanding of relapse risks. This leads to less emotional burden and allows families to focus on care and recovery rather than frequent medical appointments.
What future applications could arise from advancements in AI and MRI analysis for brain cancer treatment?
Future applications from AI advancements in MRI analysis for brain cancer treatment may include enhanced diagnostic tools, personalized treatment plans, and even the ability to preemptively administer therapies based on predicted relapse risks, thus revolutionizing how pediatric gliomas are managed.
What are the limitations of current AI models in brain cancer prediction?
While current AI models show promising results in brain cancer prediction, limitations include the need for further validation across diverse clinical settings and ensuring that the models maintain accuracy and reliability before being applied in standard patient care.
How are researchers ensuring the effectiveness of AI in brain cancer prediction models?
Researchers are ensuring the effectiveness of AI in brain cancer prediction models by leveraging large datasets of MRI scans, employing techniques like temporal learning, and conducting rigorous studies to validate model outcomes before clinical implementation.
When might AI in brain cancer prediction be applied in clinical settings?
AI in brain cancer prediction may soon be applied in clinical settings pending the success of further validation studies. The goal is to launch clinical trials to assess whether AI-derived predictions can lead to improved patient care and outcomes for pediatric gliomas.
| Key Point | Details |
|---|---|
| AI Tool for Prediction | An AI tool outperforms traditional methods by predicting relapse risk in pediatric brain cancer patients. |
| Temporal Learning Technique | The model analyzes multiple brain scans over time to improve accuracy in predicting cancer recurrence. |
| Accuracy of Predictions | The AI’s prediction accuracy for relapse is between 75-89%, significantly higher than the approximately 50% accuracy of traditional single-scan predictions. |
| Research Team and Publication | Conducted by Mass General Brigham and published in The New England Journal of Medicine AI. |
| Future Implications | Further validation is needed, but potential clinical trials may adjust imaging frequency and treatment based on AI predictions. |
Summary
AI in brain cancer prediction has shown significant promise, as highlighted in a recent study where an advanced AI tool demonstrated superior accuracy in predicting relapse risks in pediatric glioma patients compared to traditional methods. This innovative approach uses temporal learning to assess changes over multiple brain scans taken over time, ultimately aiding in better risk management and potentially improving care pathways. As research continues, the application of AI in this field could revolutionize how we understand and treat brain cancers in children.